Background:
Cancer is one of the most common causes of morbidity and mortality today with more than 14 million new cases worldwide. Oral cancer is the eighth most common cancer worldwide. Each year approximately 1 million people in India are diagnosed with oral cancers. The prevalence of cancer in India is expected to increase from an estimated 3.9 million in 2015 to an estimated 7.1 million people by 2020. India has a peculiarity in harboring world’s highest number, nearly 20% of oral cancers. The age standardized incidence rate of oral cancer is 11.2%, mortality rate is 10.2% and prevalence rate is 12.6% per 100,000 populations amongst Indian men. The projected burden of cancers among males by the year 2020 in India shows the number of cases will be lung (102,300), mouth (99,495), prostate (61,222), tongue (60,669) and larynx (36,079). Cumulatively, this makes 'oral cancer' the leading cancer site for men in most of India. Estimated number of new oral cancer by the year 2030 in India would be 1,20,127 with overall increase in incidence rates.
Oral Cancer is primarily caused by the use of tobacco and its products, which are common practices in India. Tobacco related cancers constitute 40.43% of all cancers in males. The overall survival of Indian patients with cancer is about 30% lower than the developed countries and its economic fallout is devastating. Data from regional cancer centers in India suggest that lower survival is primarily due to delayed diagnosis and presentation in late stages. More than two-thirds of patients report the cancer in an advanced stage. It is evident that most of the oral cancers are largely preventable, if detected early. But often there is a delay in diagnosis due to lack of awareness, inadequate diagnostic services, and lack of trained specialists. This results in low treatment outcomes and higher cost to patients.
Approach:
Early detection by screening is an important intervention in cancer control, especially in low and middle-income countries. There is an evidence that direct visual examination of the oral cavity is a cost effective method for oral cancer screening in resource-constrained settings. The frontline healthcare providers can help in down-staging of oral cancer and play a key role in motivating the patients to quit deleterious habits for a healthy lifestyle.
However, conventional screening has few limitations. Poor patient compliance for follow up is one of the main drawbacks. Rigid follow up to monitor the progression of Oral Potentially Malignant Disorders (OPMD) is very critical in oral cancer surveillance program. The other limitations include lack of permanent portable record of data after screening, slow rates of information transfer, poor communication between primary provider and specialist.
Intervention:
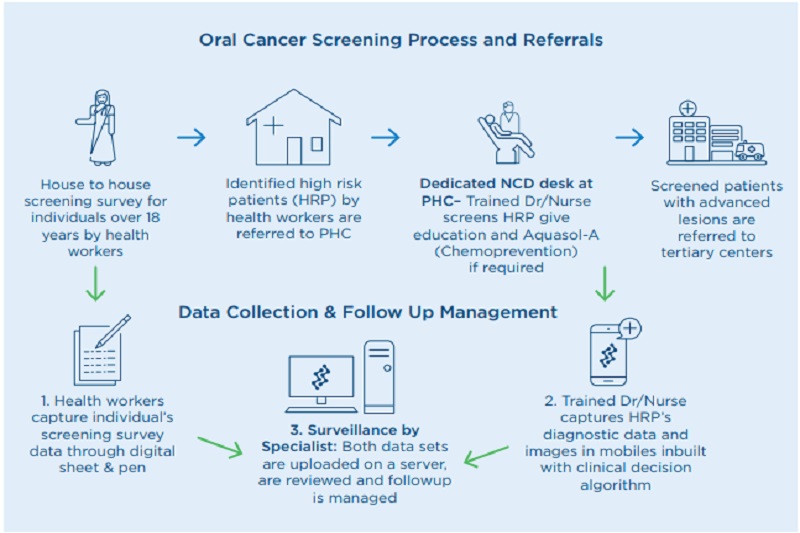
To address the shortcomings in conventional screening, Biocon Foundation introduced a mobile health (mHealth) program. The Foundation has developed and implemented a mobile phone-based management platform for cancer screening and surveillance that enables the creation of electronic health records and facilitates targeted screening for Oral Cancer. The program empowers the front line healthcare providers with mobile phone equipped with decision-based algorithm for early detection of oral cancer. This mHealth allows Electronic Data Capture (EDC) that provides a platform to connect specialists with rural population for diagnosis. It also creates an opportunity for follow up and referrals. The screening process is evidence-based, as every patient has a unique patient identity correlated with their habit history and clinically-relevant photographs. The program aims at reducing oral cancer burden and financial liabilities for the patients and improving the treatment outcome.
Started in 2011, the program has been successfully implemented in various resource-constrained settings in partnership with Governments of Karnataka, Rajasthan and Nagaland. The program was designed to identify high-risk population in both community and work place settings. It has screened about 60,000 individuals and have 13% OPMDs identified for follow up among the cases screened till the end of 2019.
Salient Features:
- Train and empower the local resource persons to detect oral pre-cancerous lesions OPMDs and oral cancer
- Connects rural population to the specialist
- Generates the high risk group data and prioritise the follow up of such patients
- Provide chemo-preventive medications for oral potentially malignant disorders
- Improve self-care and create awareness on harmful effects of tobacco usage
Publications – Biocon Foundation:
- Birur PN, Sunny SP, Jena S, K Uma, Raghavan SA, Bhanushree R, Sunitha PS, Patrick S, Kuriakose R, Malliah J, Suresh A, Chigurupati R, Desai R, Kuriakose MA. Mobile health application for remote oral cancer surveillance. J Am Dent Assoc 2015;146(12):886-894.
- Rani Desai, Praveen Birur, Suchitra Bajaj, Shubhasini AR, Bhanushree R, Shubha G, Keerthi G, Vidya Tiwari, Sanjana Patrick, Usha Hedge, Sujit Shetty, Vidya Nagabhushan, Sandeep Kankanala, Shreyas Shah. Smokeless tobacco associated lesions: A mobile health approach. The J of Contem Dent Prac 2015;16(10): 813-818.
- Suneeta Krishnan, Preet K. Dhillon, Afsan Bhadelia, Anna Schurmann, Partha Basu, Neerja Bhatla, >Praveen Birur, et al . Report from a symposium on catalyzing primary and secondary prevention of cancer in India. Cancer causes control 2015. November 2015, Volume 26, Issue 11, pp 1671-1684
- Pekka E Hänninen , Joonas J Siivonen , Eija Martikkala , Diti Desai , Timo Teimonen , Satu A Tiittanen , Paul Mundill , Chetan Mukundan , Rani Desai , Praveen Birur. A Low Resource setting Oral Lesion Screening Tool
- Rani Desai, Praveen Birur, Sangeetha, Shubhasini A R, Shubha G, Keerthi G, Naveen Kumar, Sanjana Patrick. Effect of tobacco habit on Quality of life. KLES Dental Journal 2016;5:12-14.
- John Baeten, Alexander Johnson, Sumsum Sunny, Amritha Suresh, Praveen Birur, Uma K, Deepak Kademani. Chairside molecular imaging of aberrant glycosylation in subjects with suspicious oral lesions using fluorescently labeled wheat germ agglutinin. Head & Neck. 2017;1–10.
- Arunan Skandarajah, Sumsum P. Sunny, Praveen Gurpur, Clay D. Reber, Michael V. D'Ambrosio, Nisheena Raghavan, Bonney Lee James, Ravindra D. Ramanjinappa, Amritha Suresh, Uma Kandasarma, Praveen Birur, Vinay V. Kumar, Honorius- Cezar Galmeanu, Alexandru Mihail Itu, Mihai Modiga-Arsu, Saskia Rausch, Maria Sramek, Manohar Kollegal, Gianluca Paladini, Moni Kuriakose, Lance Ladic, Felix Koch, Daniel Fletcher. Mobile microscopy as a screening tool for oral cancer in India: A pilot study. PLoS ONE 12(11): e0188440.
- Ross D. Utho, Bofan Song, Praveen Birur, Moni Abraham Kuriakose, Sumsum Sunny, Amritha Suresh, Sanjana Patrick, Afarin Anbarani, Oliver Spires, Petra Wilder-Smith, Rongguang Liang. Development of a dual-modality, dual-view smartphone-based imaging system for oral cancer detection. Proc SPIE 2018; 104860V: doi: 10.1117/12.2296435.
- Birur NP, Patrick S, Bajaj S, Raghavan S, Suresh A, Sunny SP, Chigurupati R, Wilder-Smith P, Gurushanth K, Gurudath S, Rao P, Kuriakose MA. A Novel Mobile Health Approach to Early Diagnosis of Oral Cancer. J Contemp Dent Pract 2018;19(9):1-7.
- Birur NP, Gurushanth K, Patrick S, Sunny SP, Raghavan SA, Gurudath S, Hegde U, Tiwari V, Jain V, Imran M, Rao P, Kuriakose MA, Role of community health worker in a mobile health program for early detection of oral cancer. Indian J Cancer 2019;56:107-13
- Bofan Song, Sumsum Sunny, Ross D. Uthoff, Sanjana Patrick, Amritha Suresh, Trupti Kolur, G. Keerthi, Afarin Anbarani, Petra Wilder-Smith, Moni Abraham Kuriakose, Praveen Birur, Jeffrey J. Rodriguez, And Rongguang Liang. Automatic classification of dual-modalilty, smartphone-based oral dysplasia and malignancy images using deep learning. Biomed Opt Express 2018;11(9):1-12.
Research Support (Ongoing):
- NIH 2017-2022 Low cost oral mobile cancer screening for low resource setting (NIH Project collaborative partner: Mazumdar Shaw Centre for Translational Research and University of Arizona)
- “Screen and Treat” – Oral Cancer Control program – A scale up approach in association with Government of Karnataka, Rajasthan & Nagaland, India
- AI project titled “Deep learning for oral cancer Image analysis” in association with IISc.
Research Support (Completed):
- NIH-DBT 2014-2016
A Low-Cost Simple Oral Cancer Screening Device for Low-Resource Setting (Collaborated with Mazumdar Shaw Centre for Translational Research and University of Irvine - Boston University 2014-2015
Oncogrid- A mobile health (m-Health) approach to prevention and early diagnosis of oral cancer in Rural south India (collaborated with Mazumdar Shaw Centre for Translational Research and Boston University) - Vista Dental 2014-2016
Observation of oral premalignant and malignant lesions using exogenous fluorophores and handheld fluorescent imaging (collaborated with Mazumdar Shaw Centre for Translational research and University of Minnesota) - Seimens India 2015-2016
Clinical study of the CELLSCOPE as a telemicroscopy tool for oral cancer screening (collaborated with Mazumdar Shaw Centre for Translational Research Siemens Technology and University of California, Berkeley)

